- Homepage
- Trainees
- Examinations
- Examinations by Specialty
- Histopathology
Histopathology
Part 1
Histopathology Part 1
Histopathology MCQ/EMQ Examination
Part 2
Histopathology Part 2 Examination
Histopathology Practical Examination
The practical examination is comprised of six components taken over two days:
Surgical histology
Twenty cases will be provided in 10 pairs of haematoxylin and eosin (H&E) stained slides in 20-minute slots over
3 hours 20 minutes on the second morning, and is a written component of the exam. The cases are blueprinted to the curriculum and include a balanced mixture of neoplastic and non-neoplastic material. The cases are drawn from a wide range of organ systems including upper and lower gastrointestinal tract, gynaecological tract, breast, skin, soft tissue, osteoarticular, respiratory, urological, lymphoreticular and endocrine systems. This list is not comprehensive. The cases will represent a range of difficulty from straightforward cases readily diagnosable on a single H&E section, more complex cases requiring more detailed description, differential diagnosis and special techniques, and cases not capable of diagnosis on a single H&E which should prompt an approach for further techniques, extra blocks and specialist opinions. The overall level is designed to recognise pathologists close to the end of training, such that they demonstrate an appropriate approach to independent practice. The responses will be marked centrally according to pre-determined criteria, using the closed marking system.
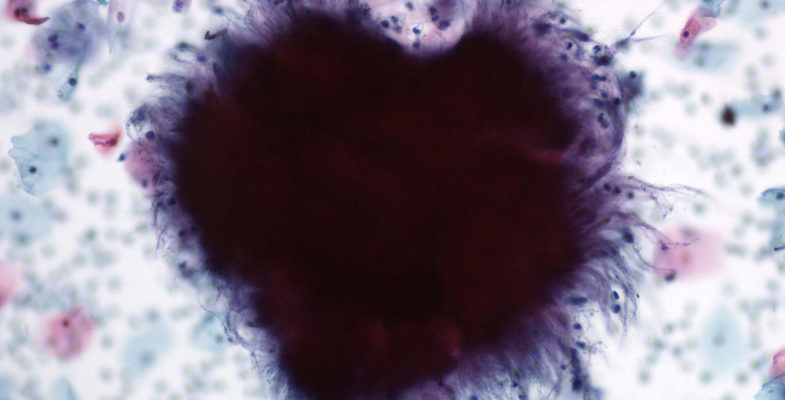
Cytopathology
8 non-gynaecological cytology cases will be provided in pairs in 20-minute slots on the first morning of the examination. The responses will be marked centrally according to pre-determined criteria, using the closed marking system. This is a written component of the examination.
Long Cases
These are 4 x 20-minute stations. They will include cases which cannot conventionally be covered by a single H&E stained section and require additional stains such as immunohistochemistry (tumours and lymph nodes), immunofluorescence (skin and renal biopsies) and electron microscopy (renal biopsies) This list is not exhaustive and other types of cases may also be used.
The responses will be marked centrally according to pre-determined criteria, using the closed marking system.
This is a written component of the examination.
Macroscopic Pathology
Four cases will be provided in the form of photographs of gross pathology specimens. Candidates will be provided with clinical information and will be asked to prepare their responses to specific questions and to mark on the photographs where they would take blocks. Two 20-minute slots will be provided to view 2 cases per slot, followed by a 20-minute discussion with 2 examiners. This section is marked on the basis of discussion with the examiners only and not a candidate's written preparatory notes. This section is designed to allow candidates to demonstrate their capabilities in discussing gross pathology and familiarity with block selection in the context of the RCPath Minimum Datasets. Each case is marked to a pre-determined marking scheme.
OSPEs
These are 2 x 20 minute stations: OSPE1 is conducted face-to-face with 2 examiners while OSPE2 is a written exercise only. Possible topics include management/clinical governance type and MDT type cases, although this list is not exhaustive.
Frozen Sections
There will be 6 cases to be viewed in 2 x 20-minute stations (3 cases per station) before meeting with a pair of examiners in a 20-minute station. Candidates should make notes, to form the basis for face-to-face discussion with 2 examiners who will expect a discussion consistent with the report given to the requesting surgeon. This section is marked on the basis of discussion with the examiners only and not a candidate's written preparatory notes.
Each case is marked to a pre-determined marking scheme.
Certificate of Higher Autopsy Training
CHAT Examination
Phase 1 - Observed Autopsy
In order to proceed to Phase 2, candidates have to satisfy examiners that they can dissect a cadaver, examine the organs, and provide a cause of death and/or a plan of further investigatory action. There is no write-up or detailed clinico-pathological questioning at the mortuary table beyond basic questions relevant to the dissection and the proposed cause of death.
Within a diet, candidates can have 2 attempts at this phase, which should take place in the candidate’s own mortuary or another where he/she wishes to be examined. The examiners should be one local consultant (perhaps the educational supervisor), and another from an adjacent region. The outcome will be pass or fail: i.e. satisfactory and proceed to phase 2 or unsatisfactory (see below).
The cadaver should be a standard case. It will not have a significant infection, complex prior operations or significantly disturbed anatomy. It will not be decomposed, or grossly obese. Medico-legal and consented autopsies are both appropriate. The purpose of this phase is to determine whether the candidate is competent at evisceration and dissection of a whole body (with APTs opening the skull but the candidate removing the brain, as in the 2005 exam format). The external examiner/s watch some or all of the autopsy dissection.
From the completion of preliminary note reading, the procedure should occupy no more than 1.5 hours for a standard case and no more than 2 hours for more difficult cases. At the end of this time, the candidate a) demonstrates the organs and normal/pathological features to the two examiners, and b) provides a cause of death and/or a plan of investigation to address the issues raised by the death. Detailed clinico-pathological discussion does not occur, and the candidate does not write the case up (unless the internal examiner so wishes, but this is not part of the examination).
The examiners decide whether or not the candidate has passed this phase and inform him/her at the time. If it is a fail, they provide constructive feedback. Only those who pass can proceed to the phase 2 OSPE session.
Phase 2 - Centralised OSPE
The OSPE examination will take place at 1 location.
The OSPE will comprise of 14 stations of 15 minutes' duration including face to face communication, written exercises and microscopy.
One or more rest stations will be applied.
The OSPE tests knowledge, skills and attitudes in various scenarios. Most are written responses and 2 are face-to-face sections. These are across 11 major autopsy pathology scenarios used variably, comprising:
- Sudden death in the community (including sudden cardiac/equivalent death)
- Medical disease and elderly pathology death
- Peri-operative death
- Toxicology death
- Medical Biochemical death (e.g. diabetes, renal failure)
- Alcohol-related death
- Special deaths (eg maternal, sickle cell, HIV, often seen in the autopsy scenarios)
- Infections (standard and atypical)
- Trauma and or suicide
- Industrial disease death
- Special tests for the autopsy, particularly data interpretation from post-mortem radiology (ie. not the images)
Using case material from these scenarios, the following aspects of knowledge and competence are examined, according to a blueprint:
- Gross pathology
- Histopathology images
- Histopathology (microscopy) in real time
- Body fluid analysis
- Communication skills
- Data interpretation
- Whole Case interpretation
- ONS cause of death formulation
- Medical-legal aspects of death
- Health & Safety issues
- Human Tissue Authority and human tissue regulations
Certificate of Higher Cervical Cytology Training
CHCCT Examination
CHCCT Examination
The cervical cytopathology examination is intended for candidates who wish to carry on and pursue higher training in Cervical Cytopathology. Successful completion of this component will result in the award of the Certificate in Higher Cervical Cytopathology Training (CHCCT).
The examination will consist of two sessions over one day.
The morning session: Twenty single slide cases over a period of 3 hours and 20 minutes on the morning of the examination. For each case a short history including the age of the patient, the stage of the menstrual cycle if known and any previous abnormal cervical cytology will be provided. Additional information may be provided if appropriate. Cases will be a mix of negative and abnormal slides. Candidates will be expected to provide a brief description of the findings on the slide and to make an appropriate management recommendation based on the clinical history and the findings on the slide. It is expected that candidates will use the terminology of the NHS Cervical Screening Programme and management suggested should be in line with current guidelines that do allow for some local variations in practice.
The afternoon session: The second paper for this examination will consist of a 2 hour written paper. The questions may include an understanding of the management of a cervical cytology laboratory participating in the National Health Service Cervical Screening Programme (NHSCSP), changes and developments within the NHSCSP, and interpretation of statistical data regarding individual and laboratory performance. It should be noted that candidates will be expected to use standard NHS Cervical Screening Programme terminology and management recommendations.