- Published:
- 18 January 2024
- Author:
- Professor Lorna Marson
- Read time:
- 9 Mins
Disparities in access and outcomes in organ transplantation are a reflection of various socioeconomic and biological characteristics. This article, by Professor Lorna Marson of the University of Edinburgh, explores the impact these inequalities have on kidney transplant patients.
Kidney transplantation is the optimal management for many patients with end-stage kidney failure. It leads to improved outcomes in terms of both quality and length of life, which can be transformational for patients and their families. In 2022–2023, 3,274 kidney transplants were performed in the UK.1 Over 5,000 patients are currently active on the kidney transplant waiting list; 63% are male.
A cornerstone of transplantation is equity of access. There is evidence of inequity by race and ethnicity, socioeconomic status, geographical location, age, sex and gender.
A recent analysis by the European Committee on Organ Transplantation of the Council of Europe outlined the landscape of the sex of donors and recipients in solid organ transplantation. The committee demonstrated that, while males are the prevalent source of deceased organs, females are more likely to be living donors and are less likely to receive a transplant than males, irrespective of the organ transplanted or whether the organ comes from a living or deceased donor.2
This article explores access to the waiting list, access to transplantation, outcomes after transplantation and patient experience. There is an imbalance between sexes in the absolute numbers of patients on the waiting list for kidney, liver, heart, and lung transplants in major international registries, such as the United Network for Organ Sharing (UNOS; US) and the Eurotransplant database. There is a greater number of females waiting for lung transplant, but more males than females are listed for all other organs.3 The reasons for this are complex and include the different prevalences of underlying diseases that lead to terminal organ failure, as well as societal factors. The focus of this article is kidney transplantation, as kidneys are the most commonly transplanted organ. The article will provide a lens through which the impact of sex on transplant patients can be observed.Females are more likely to have chronic kidney disease, but have a slower rate of progression to end-stage renal failure (ESRF) than males. Aetiologies differ: males are more likely to have ESRF due to diabetes mellitus or hypertension, while females are more likely to suffer from autoimmune disease.
The majority of, but not all, studies demonstrate that females are less likely to be listed for transplant than males. In a US study, following adjustment for confounding demographic and clinical factors, females on dialysis had 11% less access to the kidney transplant waiting list than males; importantly, older females were more affected than older males, with females between 66 and 75 years having 29% less access and females over 75 years having 59% less access than males of the same age.4 Similar findings were seen in a French study; despite access to universal healthcare, females were likely to spend significantly longer on dialysis than males prior to transplant registration. This particularly affected elderly, non-working females and females with diabetes.5 These findings were supported by work undertaken in Scotland on equity of access to the renal transplant waiting list, which demonstrated that patients were less likely to be listed for transplantation if they were female, older, had diabetes, were in a high deprivation category, or were treated in a renal unit in a hospital with no transplant unit.6 However, a subsequent analysis of access to transplantation in the UK demonstrated that recipient sex no longer remained a significant detrimental factor in terms of being listed. Other factors, such as race, age and lower socioeconomic status, persisted.7
These findings shine a spotlight on the need to interrogate the role of intersectionality in health inequalities, such as those described here. The Center for Intersectional Justice states that the concept of intersectionality describes the ways in which systems of inequality based on sex, race, ethnicity, sexual orientation, gender identity, disability, class and other forms of discrimination combine to create unique dynamics and effects. Other studies recognise the challenges posed by intersectional health inequalities, highlighting that obese females were less likely to be listed for transplantation than obese males.8 A strong association between race and access to kidney transplantation has been demonstrated in studies from the Southern US9 and Canada.10
Once listed, the reasons for whether a patient is offered an organ are complex. Females are more likely to be sensitised to human leukocyte antigens owing to previous exposure in pregnancy. This makes them less likely to be able to receive a spousal living donor kidney transplant and causes difficulties when matching for deceased donor transplantation.11 A recently published study from the UK sought to determine barriers to living donor kidney transplantation (LDKT) in a cohort of 807 recipients of kidneys from living donors; the study demonstrated that there was a significant reduction in the likelihood of LDKT for older ages, Asian and Black ethnicities, divorced, separated or widowed individuals, people with lower levels of qualifications and those who did not own a car or a home. Sex was not an independent risk factor, which highlights the biological and societal complexity of these issues.12
Early studies of sex differences in kidney allograft survival reported conflicting results that depended on the age of the study cohorts, giving rise to the consideration that sex differences in outcomes vary with age. This led to interesting work that examined the association between recipient sex and kidney graft failure by recipient age and donor sex. This was first based on the Scientific Registry of Transplant Recipients (SRTR)13 and subsequently on the 3 major transplant databases globally. Patients were based in the US and Canada, Australia, New Zealand and Europe, and included recipients from the UK. A total of 438,585 patients were involved.
Female recipients aged 0–12, 13–24 and 25–44 had significantly higher rates of graft loss with male donors than male recipients did. When the donor was female, there were no significant differences by recipient sex for those aged <45 years (Figure 1). Above the age of 60, graft survival was better for females than males, irrespective of donor sex.14
Figure 1. Age-specific hazards in kidney transplants.
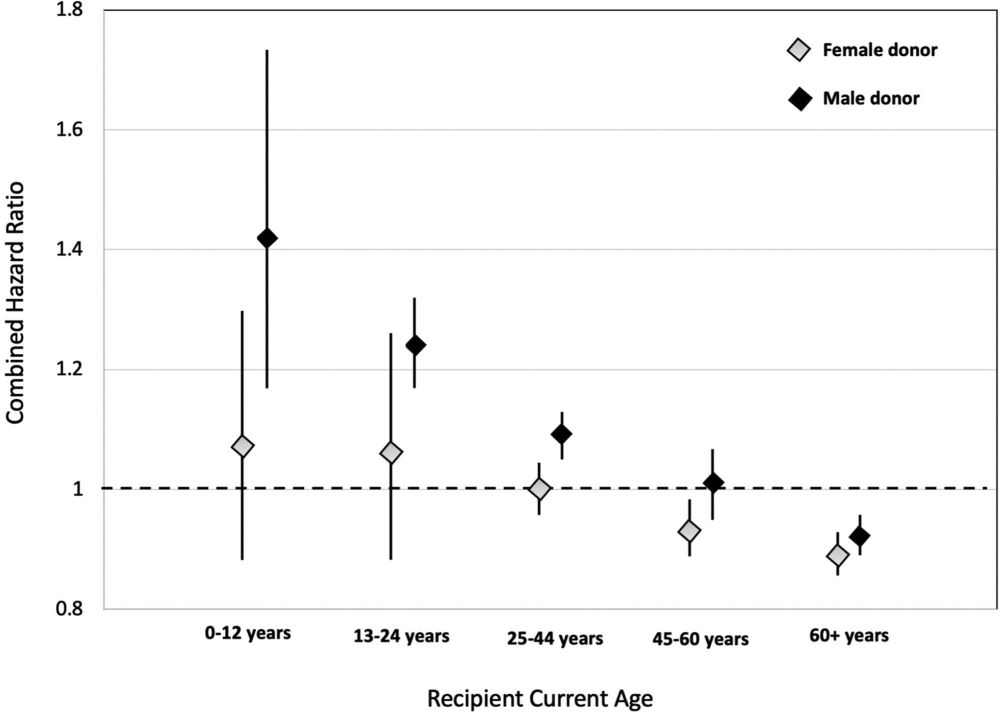
This interesting data supports the concept that there is a complex interplay between donors and recipients, which is impacted by hormonal changes, genetic factors and potential differences in drug metabolism. Oestrogen enhances immune reactivity, which is age-dependent, while testosterone has the opposite effect. Intrinsically, female patients have enhanced immune reactivity due to increased X chromosome gene expression and recognition of the HY-antigen. Data suggests that female transplant recipients are more likely to adhere to medication than males beyond the age of 16. But the pharmacokinetics of some immunosuppressive agents, such as calcineurin inhibitors, yield lower trough levels in females, making them more susceptible to rejection.15 Many drug trials exclude females, particularly those of childbearing age, so have not previously highlighted such differences.
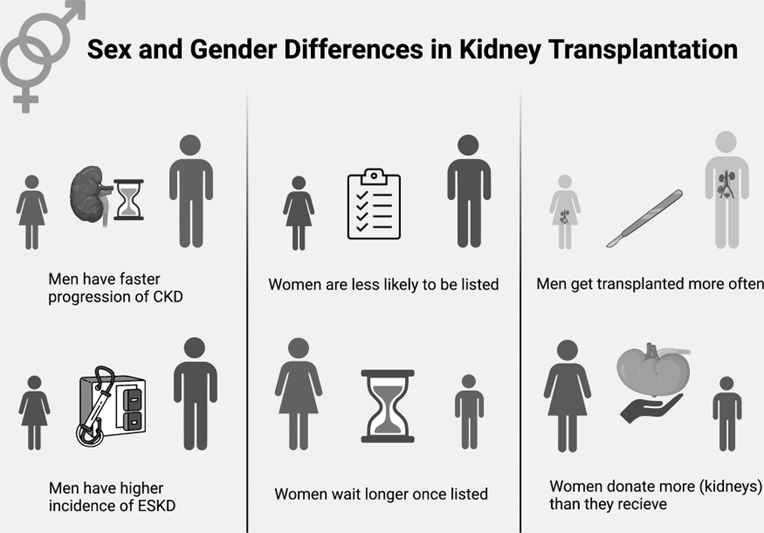
This review has focused on the differences in access to waiting lists for transplantation and to living donor kidney transplantation, as well as the different outcomes between male and female patients. The findings are summarised in Figure 2. The aetiology is complex, incorporating biological effects, such as hormonal and genetic differences, as well as societal effects. The different roles traditionally adopted by females may affect their chance of being listed for transplantation. In addition, medical professionals may demonstrate bias by adopting the traditionally patriarchal approach to medical care, perceiving females as more frail and less likely to wish to be transplanted. This is reflected in recent patient feedback from personal communications, which highlighted a lack of understanding or interest in the challenges female patients faced post-transplant, particularly but not exclusively around their reproductive health.
Figure 2. Sex and gender differences in kidney transplantation.
It behoves us to seek to improve our understanding to address these societal inequities, always bearing in mind that sex is by no means the only characteristic that impacts patient care and outcomes.

