- Published:
- 07 September 2023
- Author:
- Teresa Cutino-Moguel & Anna Riddel
- Read time:
- 10 Mins
Although the invention of vaccination has been credited to Edward Jenner, variolation (or inoculation) is thought to have originated in China or India in the 1500s (with earlier suggestions of 1000 AD). Owing to its low mortality and success in preventing fatal disease, the technique had travelled worldwide by the 17th century. Variolation was also known as ‘buying the pocks’, where pocks (smallpox scabs) were bought and inoculated into the skin using a needle, or sometimes held in the hand or tied around a child’s wrist.1
Inoculation against smallpox in milkmaids
Edward Jenner built on this success. He observed that milkmaids with cowpox infection did not develop smallpox; through a series of experiments, Jenner demonstrated that inoculation with material from a milkmaid’s cowpox sore lead to protection against smallpox (1796).2 This was the ‘first’ vaccine.
Although the term ‘vaccine’ derives from ‘vacca’,meaning cow in Latin, the origins of vaccinia, theorthopoxvirus in the smallpox vaccine, is debated.Jenner himself thought cowpox may have beenderived from horsepox. Recent sequencing analysis of a 1902 smallpox vaccine virus supports this,demonstrating a higher degree of similarity to horsepox than cowpox.3 Despite opposition from religious leaders, who suggested that the vaccine interfered with God’s will, and others who opposed the vaccine as it had been derived from animals, in 1853 the Vaccination Act made smallpox vaccination in England and Wales mandatory for infants up to 3 months old.
Subsequent advancements
Louis Pasteur was responsible for the next major vaccine development. He produced the first live attenuated rabies virus vaccine in 1885 (although the aetiological agent was unknown) from the spinal cords and brains of infected rabbits.
In 1918, the Spanish Flu pandemic made an influenza vaccine a worldwide priority. However, it was not possible to identify the aetiological agent until the invention of the electron microscope in the 1930s. This enabled investigators to visualise influenza and other viruses, paving the way for further vaccine development. The yellow fever vaccine followed shortly after in 1939. The first successful influenza virus vaccine was produced in 1945. See Figure 1 for a timeline of vaccine development.The creation of the World Health Organization (WHO) in 1948 led to reframing of public health as a global problem. Smallpox and poliovirus were identified as targets for elimination, theoretically possible as neither have an animal reservoir.
Since the 1964 establishment of the global Essential Programme on Immunisation, many new vaccines have been introduced, like the hepatitis B, rotavirus and human papilloma virus vaccines.
In the developing world, vaccine uptake has been slow in some regions. For example, in areas of high hepatitis B incidence in Africa and Southeast Asia, it has taken more than 20 years to introduce routine HBV vaccination (WHO).4
Global coverage of HBV vaccination is nearly 80%, which has benefited from a lower cost and incorporation in the pentavalent vaccine.
Eliminating smallpox
In 1967, the WHO announced the Intensified Smallpox Eradication Programme to eradicate smallpox in more than 30 countries using surveillance and vaccination. Through an unprecedented global coordination, the eradication of smallpox was declared in 1980. This marked the first globally significant success of the WHO since its conception and remains ‘one of the most notable and profound public health successes in history’.5
Vaccinating against polio
The first effective polio vaccine was developed by Salk in 1952. At this time, there were around 8,000 poliomyelitis cases each year in the UK6 and worldwide, with paralysis or death in half a million people each year (WHO).4
In 1988, the World Health Assembly passed a resolution to eradicate polio, launching the Global Polio Eradication Initiative. Although 2 of the 3 serotypes of poliovirus (types 2 and 3) have been successfully eradicated, serotype 1 still circulates in Pakistan and Afghanistan with regular spread to neighbouring countries.7
Figure 1: Flowchart of the history of vaccine development and British routine vaccine programmes.
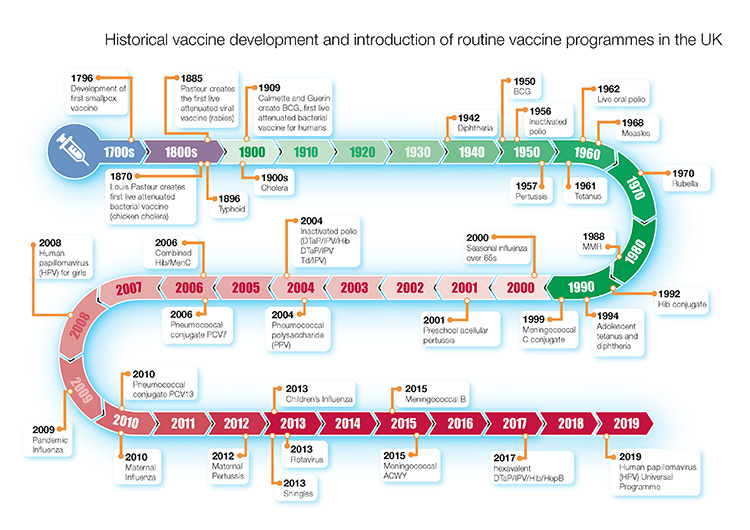
Source: UK Health Security Agency. Contains public sector information licensed under the Open Government Licence v3.0.
There has been a 99.9% reduction in the number of polio cases since the beginning of the eradication programme, with 400 cases reported in 2013. As of July 2021, only 2 cases of wild poliovirus were recorded globally: one in Afghanistan and one in Pakistan. Despite this success, challenges to polio eradication remain. Circulating vaccine-derived polioviruses (VDPVs) from oral polio vaccines are a threat, as they can acquire mutations which lead to reversion to neurovirulence. In the UK in 2022, VDPVs were detected in routine sewage testing between February and July 2022.8
Detection of VDPVs in isolated samples is not rare but, in this incident, several samples were positive with closely related type 2 polioviruses indicating person-to-person transmission in the community. This is possible in countries where there is inadequate vaccination or where inactivated poliovirus vaccines (IPV) are used for routine childhood vaccinations like the UK, as the IPV does not provide mucosal immunity, meaning person-to-person transmission is possible. Unvaccinated people will be susceptible to infection with potential for subsequent disease.
A remaining threat from measles
The measles vaccine has led to an estimated 73% reduction in measles mortality between 2000 and 2018 and prevented 23.2 million deaths (WHO).9 However, measles remains a public health threat in every region of the world. Measles vaccination uptake has declined since the beginning of the COVID-19 pandemic, with nearly 40 million children missing their first or second doses in 2021.
During January and February 2022, 17,338 measles cases were reported worldwide, compared to 9,665 in the same period of 2021. This 79% increase in cases has raised alarms about the significant disruption that routine immunisation suffered during the pandemic, with further complications created by displacement and conflict in countries like Ukraine, Ethiopia, Yemen, Somalia and Afghanistan.9
Even in the UK, where the MMR vaccine is part of the routine NHS childhood vaccination schedule, a rise in measles cases has been reported; between 1 January and 20 April 2023 there have been 49 cases compared with 54 during all of 2022.10Safety
We still face many other challenges in the development and roll-out of vaccines. Vaccines need to be very safe, as well as effective; they are given to prevent diseases when a person is well, so side effects need to be minimal. The demonstration of safety and efficacy in animal then human clinical trials can take years and billions of dollars of investment.
In addition to limiting side effects, we do not understand which are the appropriate or optimal antigenic targets for vaccines in many infections. Similarly we do not have widely available standardised diagnostic tests to provide a good understanding of vaccine-induced immunity and the correlates of protection for some infections.
Efficacy
Many pathogens targeted by vaccines are a moving target, owing to antigenic mutations and diversity and differences in host immune responses (genetic and environmental). These issues pose challenges for developing an effective vaccine for a global population. Similarly, identifying the appropriate mode of delivery to ensure immunity is developed at a primary site of interaction with a pathogen is challenging. Vaccines that lead to mucosal immunity are limited but are thought to be necessary to prevent transmission/infection in respiratory and gastrointestinal pathogens where parenteral vaccines mostly attenuate severity of infection only (influenza, COVID-19, IPV).
Delivery and acceptance
Even if safe and effective vaccines are developed, a significant obstacle to vaccine delivery in low and middle-income countries remains the storage and handling conditions required. Prolonged cold chain requirements can be problematic, owing to unreliable electricity supply and/or lack of refrigerators. Political instability and conflict have already been mentioned as a cause of disruption of the measles vaccination programme in many countries.
Today, there is the largest population of forcibly displaced people ever – an estimated 103 million people, with 50% being internally displaced.11 74% of refugees are hosted in low- and middle-income countries. Owing to this displacement, many of these people will not have received appropriate vaccinations. We may well see a resurgence of vaccine-preventable diseases in countries where eradication was reported previously (e.g. diphtheria in the UK in 2022).
Strongly held beliefs can deter people from being vaccinated and misinformation spread through social media can have an enormous power on these beliefs. This was the subject of last year's RCPath Book Club webinar, in which Professor Heidi Larson discussed her book Stuck: How Vaccine Rumours Start and Why They Don't Go Away – still available to view on the College website.This is an unequal world. In the 1990s, almost 30 million children in developing countries were not fully immunised or immunised at all. Although vaccines were available, developing countries could not afford them. In response to the global disparity in vaccine accessibility, the Global Alliance for Vaccines and Immunisation (GAVI) was created in 2000. The aim was to encourage manufacturers to lower vaccine prices for the poorest countries in return for long-term, large and predictable demand for vaccines from these countries. This initiative is calculated to have prevented 13 million deaths.
The Coalition for Epidemic Preparedness Innovation (CEPI) was launched at Davos in 2017 following the Ebola virus epidemic in 2014, which caused 20,000 deaths and an estimated economic and social burden of $53.19 billion to the affected countries in West Africa.12 This global partnership between private, public and civil society organisations was formed to accelerate the development of vaccines against emerging infectious diseases, as well as ensuring equitable access for affected populations.
Alongside GAVI, other agencies including the WHO, the United Nations Children’s Fund, the Vaccine Alliance and CEPI have been fundamental for the expansion of vaccination programmes worldwide. This was particularly evident during the COVID-19 pandemic. Vaccination was demonstrated to be a community activity, where vaccination of some can protect others and vice versa.
Vaccines have prevented approximately 6 million deaths annually and save 386 million life years and 96 million disability-adjusted life years globally.13 Healthcare interventions are cost-effective if they provide a year of healthy life for less than the per capita gross national product (GNP) in a country. Most low-income countries have a GNP of $765 or less and vaccines in the EPI programme cost less than $20 per year of healthy life gained from them. By comparison, hypertension treatment in the USA costs between $4,340 and $87,940 and treatment of 1 case of measles costs 23-times the cost of vaccinating a child. In developing countries, the cost of immunising millions of children against polio, diphtheria, pertussis, measles and tetanus is similar to the cost of a single day of healthcare in the USA.13
Additional benefits of vaccination exist even when they can be difficult to quantify. Vaccination activities can facilitate interactions with the community where other health issues are dealt with, such as provision of contraception methods or vitamin supplementation to combat malnutrition.14In the UK there is a comprehensive routine vaccination programme delivered by the NHS.15 Vaccination and health prevention strategies have a positive impact on healthcare. They reduce hospitalisation for acute infections and their short- and long-term complications. This was particularly evident during the COVID-19 pandemic. The first dose of a COVID vaccine outside of a clinical trial was given in December 2020. Worldwide, 70% of the world population has had at least 1 dose of a COVID-19 vaccine, although only 30% of people in low-income countries. Around 13.38 billion doses have been given worldwide.16
The Early Pandemic Evaluation and Enhanced Surveillance of COVID-19 (EAVE II) stated that the countrywide effect of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines in the community was to prevent hospitalisation from COVID-19 by up to 85% and 94%, respectively. Even after the emergence of SARS-CoV-2 variants, a booster dose increased protection against hospitalisation by 50 to 60%.17
Globally, it is estimated that COVID-19 vaccines prevented 14.4 million deaths in 185 countries in the first year since their introduction. This increases to 19.8 million when excess deaths are calculated. Nevertheless, the failure to achieve the 40% coverage target set by the WHO prevented vaccines from exerting their maximum benefit, with millions of lives lost as a result.18
Although vaccines have the increasing potential to change or eradicate many diseases that afflict humanity, this is fully dependent on equitable and fair access in our globalised world.
Return to July 2023 Bulletin homepage





