No one can fail to see how better use of data could transform healthcare; the management of blood components is no exception. Blood transfusion is the most common intervention in hospitalised patients: nearly 2 million blood components are issued and transfused in England at an estimated cost of over £300 million per year. The evidence base for transfusions and related alternatives has expanded considerably; recommendations for safe and effective use have become stronger, supporting restrictive usage.
Concerns in transfusion services
Yet, audits and studies of practice continue to indicate that up to 20% of blood is used outside evidence-based recommendations.
These observations raise important questions.
- Are patients being exposed to risk from unnecessary transfusions?
- How can we best ensure clinicians and healthcare professionals use blood according to evidence-based guidance?
The other aspect of concern is the supply of blood for transfusion. Blood is collected from volunteer donors, either as whole blood or by apheresis. There are no financial incentives offered and donation is a purely altruistic decision. All blood transfusion services, therefore, operate on a fine-tuned supply model, adapted to meet demands and also to avoid wasting this precious resource.
Indeed, this balance of supply and demand can be quite readily perturbed. Stocks of most blood components are generally only sufficient to cover short periods of a few days or up to a week.
During the COVID-19 pandemic, there were real concerns that during lockdowns, blood donations would fall to unacceptable levels and, more recently, NHS Blood and Transplant (NHSBT) declared blood supply alerts (see the article on the blood shortage in the January 2023 Bulletin).
New initiatives to ensure transfusion safety
Transfusion 2024
Several major initiatives have begun to address these concerns. The first is Transfusion 2024, a strategic plan developed in collaboration with the National Blood Transfusion Committee and NHSBT, supported by NHS England. The plan outlines the key priorities for clinical and laboratory transfusion practice to enable safe patient care across the NHS. The aim is to improve patient outcomes by enhancing and delivering the necessary infrastructure to support good transfusion practice.
A programme of change has started and includes projects that will focus on addressing variation in transfusion practice and concerns around the delivery of services from hospital transfusion laboratories to support safe transfusion. The need for integrated IT systems is critical to enable rapid, good-quality data exchange.
Research into transfusion data
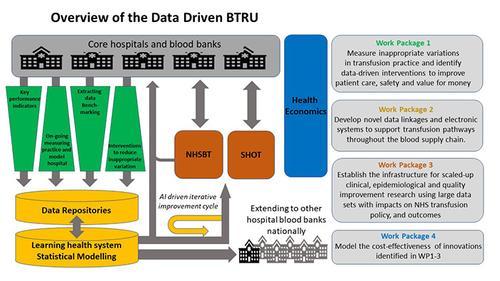
The second initiative centres around a new infrastructure research unit – Data Driven Transfusion Practice – which was launched in 2022. It is 1 of 5 Blood and Transplant Research Units (BTRUs) that have been created in a £20 million programme, co-funded by the National Institute for Health and Care Research (NIHR) and NHSBT (see the article in the July 2022 Bulletin).
This particular research unit, hosted by the University of Oxford, will strengthen and enhance data-driven approaches. Actual data will be used in all steps in the transfusion chain to offer new ways to improve transfusion practice and decrease the rates of inappropriate blood usage.
The Data Driven Transfusion Practice unit
Here, we provide 3 examples of the projects within the BTRU to exemplify how this approach will drive innovation and improvement.
Addressing variation
It is essential to start by understanding the variation that is currently occurring in transfusion practice across the country. Routinely collected hospital and primary care data will be used to identify the variations in blood usage that occur between different hospitals, patient groups, procedures, etc. In principle, this should allow a better understanding of the reasons for variation and assist with the design of improved practice. Currently, however, there is a lack of data integration across hospitals to enable visibility across the whole blood supply chain. The individual IT systems and dispersed nature of the data can make even the transference of data within an individual trust a complex process. This is further complicated by the fact that individual trusts broker their own agreements with IT suppliers, which means the opportunities for mass applicable adaptations is not simple.
To understand what each hospital needs in what circumstances, we need a better picture of how blood moves around the system in response to what stimuli and to be able to interrogate that data in as near to real time as possible. Online shopping stores like Amazon manage their stock in an amazing way – but we are a long way from that ideal. The data used to monitor traceability is a good starting point, but there is work to be done to connect the sometimes very disparate informatics systems. The BTRU will work on a range of projects aimed at better and faster data tracking through upgraded data collection and system interoperability. We are starting to gather a more complete understanding of the state of electronic systems within the UK so future planning can be done in an informed way to build the ultimate electronic vein-to-vein pathway. Our first example in this has been a peri-operative survey of IT capability during surgery, planned with the Research and Audit Federation of Trainees, a network of regional groups of Anaesthetic Trainee Research Groups.
Data repositories
The second approach is to create and analyse large-scale datasets that include information on anaemia and transfusion status. This will allow the examination of the consequences of anaemia or transfusion in various disease models and produce feedback on when and where it creates additional benefit or risk to patients. One example of this is work within perioperative care at the Nuffield Orthopaedic Centre in Oxford. This project will be later used to develop prediction tools to better identify which patients undergoing orthopaedic surgery will experience adverse events or complications. By identifying those at the greatest risk, more personalised blood management strategies can be developed, tested and employed to improve patient outcomes and reduce healthcare costs.
Enhancing feedback
These days, clinicians are overwhelmed by data and have little time to process it all. It’s incumbent to provide feedback information on practices as clearly and quickly as possible to the correct individuals at the right time. Not only do we need to provide the most up-to-date data, but it is also important to be aware of the data burden on the clinical team and ensure the appropriate information is provided to the right person.
We must always consider how information is delivered to clinicians in an impactful way to ensure that practices are aligned with best recommendations, for example, in guidelines. This includes the question of how data should best be presented to achieve impact (data visualisation). Working alongside the University of Leeds, we aim to evaluate and identify more effective means of communicating findings to clinicians and changing practices. For example, with established audit processes, we have already identified ways in which regular reporting, like that providedon stock levels from the NHSBT Blood Stocks Management Scheme team, can be optimised to increase impact.
This will go hand in hand with our work to understand the people and teams using this information and, in the long run, provide a source of information for the development of the model hospital dashboard-style feedback approach.
Reducing inequality
The work of the Data BTRU is closely monitored and driven by the opinions of our public and patient contributors. Drawn from a wide cross-section of the population, these volunteers have raisedquestions about how outcomes can be affected by different biases, for example those linked to postcode, ethnicity or socioeconomic status.
In all our work, we recognise that our data may initially come from more privileged hospitals and sites, however defined. This presents the possibility that we could risk the amplification of inequality unless we are careful about how we interpret that data. To overcome this, it is important to be clear about where the inequality lies.
Data recording varies. For example, different hospitals across the UK use different Office for National Statistics categories for what should be standard data, such as ethnicity. Many studies have chosen not to record ethnicity data at all, meaning that any assessment of health inequality cannot be reported.
An examination of our population demographics, as well as the acknowledgement of poor recording or absent data, must be highlighted so further studies can act to address this going forward. We intend this to be a major output of this data programme.
Costs and benefits
Finally, we are collaborating with Barts and the London School of Medicine and Dentistry to investigate the costings of different pathways and processes for transfusion, right through from donor vein to recipient vein. By identifying these costs, we can establish what savings and benefits might be achieved through using electronic data or electronic systems for blood transfusion more widely. For example, some 2-person checks, necessary under current protocols, may become redundant with electronic systems, saving valuable clinical time and cost.
In the short term, both the Transfusion 2024 and BTRU-data programmes may be able to achieve some quick wins. For example, by using better electronic systems to improve e-requesting and reporting and possibly remote interpretation of samples by NHSBT centrally to support staff in hospitals. This is being piloted but it is still early days to decide on its economic viability.
Looking further into the future, it may be possible to use remote technology, similar to Fitbits or smart watches, to better monitor patients who are dependent on regular transfusions. Again, this will help with the move towards personalised approaches to transfusion practice. This might not be only for complications of blood transfusion, but also to help identify the efficacy of treatment related, for example, to outcomes like patient activity. Ultimately, we may also be able to use remote technology to enable safe transfusions at home, thus reducing costs and resources.
In the end, saving a bag of blood for transfusion through prioritising electronic interventions does not just save the nominal cost of that bag, but of the whole infrastructure used to collect, save, transport, monitor and transfuse it. Saving a bag of blood to avoid unnecessary transfusions is not just about reducing the economic cost of treatment, it ensures the availability of blood, a scarce resource, for patients who really need transfusions, such as for major bleeding, and it also helps patients’ long-term wellbeing and quality of life.






