Results of three surveys (local, regional and national) of blood culture practice were published in the College Bulletin in 2015.2 These surveys highlighted improvement opportunities to build on existing practices in the blood culture pathway to improve patient care and outcomes. The conclusion highlighted that the adoption of ISO 15189 standards by clinical pathology accreditation, along with the recommendations of the Pathology Quality Assurance Review chaired by Ian Barnes,3 encourages laboratories to monitor end-to-end processes as markers of overall quality.
In accordance with recommendations from the Shape of Training report,4 the infection specialties have evolved to develop more patient-focused care. However, financial, workforce and operational constraints can pose a challenge for diagnostic laboratory services. Board, ward and laboratory leadership must work together to provide the best support and deliver optimum patient care throughout the blood culture pathway.
NHS England’s report into blood culture practices
In 2022, NHS England published a report into blood culture practices1 that outlined the key improvement steps needed in the pre-analytical phase of the blood culture pathway.1
The report includes results from NHS England’s nationwide survey of blood culture practices against SMI B37 standards, 2018–2019, which highlight the need for a board-to-ward-to-laboratory approach.
Drawing on the survey results, the report includes four key recommendations to optimise the blood culture pathway. These do not change the standards set out in SMI B37, but outline the key actions required to support pathway improvement:
- build upon existing national guidance and best practice
- implement local monitoring to identify areas for improvement
- antimicrobial resistance (AMR) must be a core part of clinical leadership and Trust governance
- improve regulation assessment and accreditation assessment of end-to-end pathways.
These recommendations present an opportunity for the NHS to be global leaders in improving blood culture practices, antimicrobial stewardship and patient outcomes from sepsis.
Adopting existing current blood culture guidance Guidance and an accreditation process (ISO 15189, UKAS) are in place for blood culture practices.5 However, areas for improvement have been identified:
- ensuring that wherever possible, the right volumes of blood are collected; the lower the volume, the lower the chance of detecting organisms causing an infection.
- ensuring that samples reach the analysers as quickly as possible. Most patients with infections will have blood cultures that will signal positive within 12 hours of collection (generally 6 hours onwards) in an optimised pathway. In addition, keeping the timeframe from ward to analyser as short as possible also preserves sample integrity, maximising the chances of detecting infection.
Several staff groups are involved in achieving this and, therefore, the essential steps required to improve the pathway require a board-to-ward-to-laboratory collaborative approach.
Local monitoring to improve your blood culture pathway
As part of the NHS England report, regular audits are recommended as a way of maintaining and improving quality across the blood culture pathway. Due to the distinctive biological variability between blood culture sets, there is no standard time it takes for a blood culture to signal positive. Without audit, it is impossible to determine whether the blood culture pathway is functioning in the best way. Audit is the key first step to improving the pathway by giving an understanding of any local challenges and how these can be addressed through a board-to-ward-to-laboratory approach. This approach is key, as many aspects of the audit require collaboration across the teams who collect and deliver the samples to the diagnostic laboratory. If we can’t measure it, we can’t improve it.
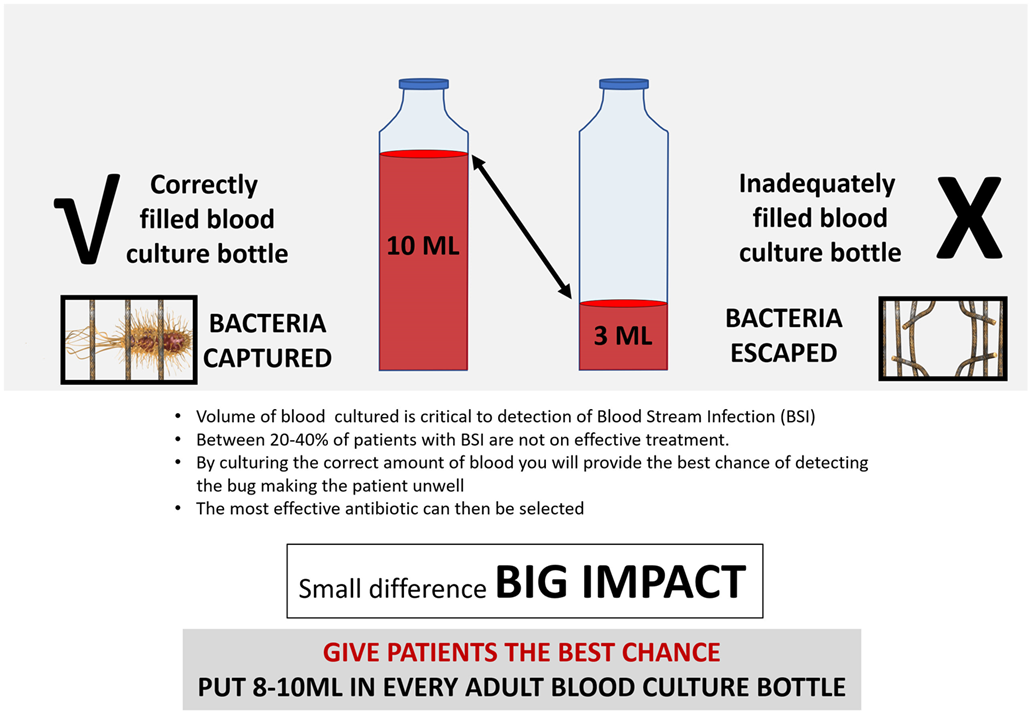
Figure 1. Illustration of correctly filled blood culture bottle. 8–10 ml of blood is required to best detect bacteria.
Multidisciplinary working
Samples should not be viewed as a laboratory test alone; the end-to-end pathway should be the focus. Otherwise, the pre-analytical and post-analytical phases of the pathway may not provide optimal care. Executive teams and trust boards must work together to ensure that optimised pathways are being followed. It is crucial to support this initiative to improve patient care and patient safety.
Updating accreditation
Patient focus must be at the forefront of accreditation assessments. Without this, there is a risk of quality becoming disconnected from the objective of improved patient care.6
Accreditation assessments need to be undertaken in such a way that deficiencies in this pathway (and any other clinical pathway) are identified as swiftly as possible, so improvements can be made with the right support.
The patient impact of improving blood culture practices
Early identification of blood stream infections (BSI) supports a more accurate infection diagnosis, reduced length of stay and more appropriate prescribing. Patient flow would improve within hospitals as patients are put on the appropriate treatment pathway as quickly as possible. This all contributes to the drive to improve antimicrobial stewardship and, ultimately, patient care. A recent multicentre study on the patient impact of inappropriate empirical antibiotic therapy (as judged by laboratory sensitivity testing) for BSI concluded:
- approximately one in five patients with BSI received inappropriate empirical antibiotic therapy, which has been associated with increased mortality overall, even in patients without sepsis
- early identification of BSI and resistance improves patient and population level outcomes.5,7
By collecting the right volume of blood from a patient and incubating the samples in a blood culture analyser in a timely way, we can detect BSI in adults faster and more accurately and treat those with sepsis at the speed required.8,9 NHS England recommends two blood culture sets of 8–10 mL per bottle, illustrated in Figure 1, with sample bottles incubated in a blood culture analyser within a maximum of four hours.
What is the role of blood cultures when tackling antimicrobial resistance? Missed opportunities to audit and optimise the blood culture pathway risks rising mortality from sepsis. In addition, as failure rates of empirical antimicrobial therapy increase along with fewer effective antibiotics being available, due to increasing AMR, antimicrobial stewardship becomes even more important. The effectiveness of these remaining antibiotics is likely to diminish if delays occur in putting patients on the appropriate therapy, for example, due to delays in the blood culture pathway or a pathogen not being identified due to a falsely negative blood culture.
Raising the bar for pathology Specimen pathways are central to effective patient care and pathology plays a pivotal role in improving patient outcomes, reducing length of stay and fighting back against AMR. To ensure the best result for our patients, any silo working focusing on the laboratory phase alone must change. Pathology working alone cannot deliver successful pathways. It requires a multidisciplinary team approach, with targeted education and the appropriate governance and recording mechanisms in place to audit, monitor and report on performance against the necessary standards. Pathology has a lot to offer to benefit patient care and protect the public health of the population.
For further information, please contact: [email protected].
References available on our website.
Comment from the College
The College welcomes this important initiative to improve the blood culture pathway. It will undoubtedly positively affect patient care and experience. However, as the upcoming College workforce report illustrates, significant workforce shortfalls within medical microbiology pose a challenge to its success. Many of the changes required to implement this fall outside of the remit of the medical microbiologist and diagnostic laboratory. For example, multidisciplinary teams are required to ensure there is sufficient volume of blood inoculated into blood culture bottles and prompt transport to the laboratories following venepuncture to ensure the time to loading onto analysers is optimised.
To achieve this, the College supports a board-to-ward-to-lab approach with Trust leadership establishing AMR as a core part of clinical leadership and trust governance.
Natasha Ratnaraja
Chair, Medical Microbiology/Medical Virology SAC
Professor Angharad Davies
Vice-President (Learning)