I am a haematology registrar training at King’s College Hospital. I work with patients with a range of blood disorders including blood cancer. During the COVID pandemic I was working at the Princess Royal University Hospital, Farnborough, where I was redeployed to support COVID-19 patients in the respiratory high-dependency unit.
Our haematology inpatients are some of the most vulnerable to infection in society and therefore we were all doing our upmost to shield them.
My blog is a personal account of how I used my haematology skills during my redeployment and what I found when I returned to working with blood cancer patients.
Redeployment
Well, it has been a strange year, that’s for sure. Personally, my first brush with COVID-19 was getting it myself in mid-March. I was unwell with high fevers and a cough for a few days and a week later was back at work. I was only back a week when I heard that, from the beginning of April, I was being redeployed to the newly formed respiratory high dependency unit (HDU). As I had worked in intensive care before, I was going to be a respiratory HDU registrar! I will admit I was extremely nervous, both because I had not done any respiratory medicine or intensive care medicine for several years; and also because we knew the peak of infections was due to hit our hospital that weekend.
To be honest, I was scared about what I might have to face in the coming weeks. However, the respiratory physicians I was working with were wonderful, excellent at their job, kind and approachable. The first week I was providing a respiratory outreach service with a consultant and a specialist nurse, Nicky. We went from ward to ward assessing the sickest patients suffering from COVID pneumonia and moving them to HDU. It seemed like there were endless wards of patients with the same symptoms.

Once I got used to the respiratory side of things, I realised that a lot of my skills as a haematologist were being used.
When I started working in the HDU itself the physical toll of working in full PPE - mask, hat, visor, long sleeved gown and gloves - hit me. The gowns were always XXL in size, difficult to move around in, it was hot and sweaty and hard to hear each other talk, let alone hear the patients who had on oxygen masks or CPAP machines. We tried to go into the sealed unit for four hours at a time to minimise wastage of precious PPE. The hardest thing was that the patients could not have their loved ones with them. I had to have a lot of difficult and heart-breaking conversations over the phone. We tried to arrange for families to video call whenever possible, particularly if the patient was about to be put onto a ventilator. Some of these experiences will always stay with me.
Using my skills as a haematologist in the HDU
Once I got used to the respiratory side of things, I realised that a lot of my skills as a haematologist were being used. Patients were being faced with a scary diagnosis and uncertain treatment and I tried to explain to them what was going on in a way they could understand. The whole multidisciplinary team worked well together, doctors, nurses, respiratory physios, specialist nurses, palliative care specialists and occupational therapists. Working in the HDU was a high-risk environment for staff and I was so impressed by everyone just getting on and doing their jobs for the benefit of the patients.
Towards the end of my time in respiratory HDU, some of the patients who had gone to intensive care started to come back to the ward on their journey to recovery. This was such a positive moment for us all, in particular the nurses who had spent long hours nursing them when they were so sick. I enjoyed seeing patients require less of my input and more of the physios and occupational therapists as they learnt to walk again and regained their strength. They received a big round of applause when they left the ward!
Whilst redeployed, I became involved with the clinical trials team and helped to recruit patients to trials looking for a treatment for COVID-19.
Clinical Trials
One of the things I like about being a haematologist is that we have access to cutting edge treatments for some of our patients and many of them are enrolled in clinical trials. This is an area I hope to work in in the future. Whilst redeployed, I became involved with the clinical trials team and helped to recruit patients to trials looking for a treatment for COVID-19. This included the RECOVERY trial which is ongoing but is leading the way globally in trying to find effective treatments for people hospitalised with COVID-19. For me, this was a great link between haematology and my redeployment to the COVID wards.

My return to haematology - impacts on blood cancer patients
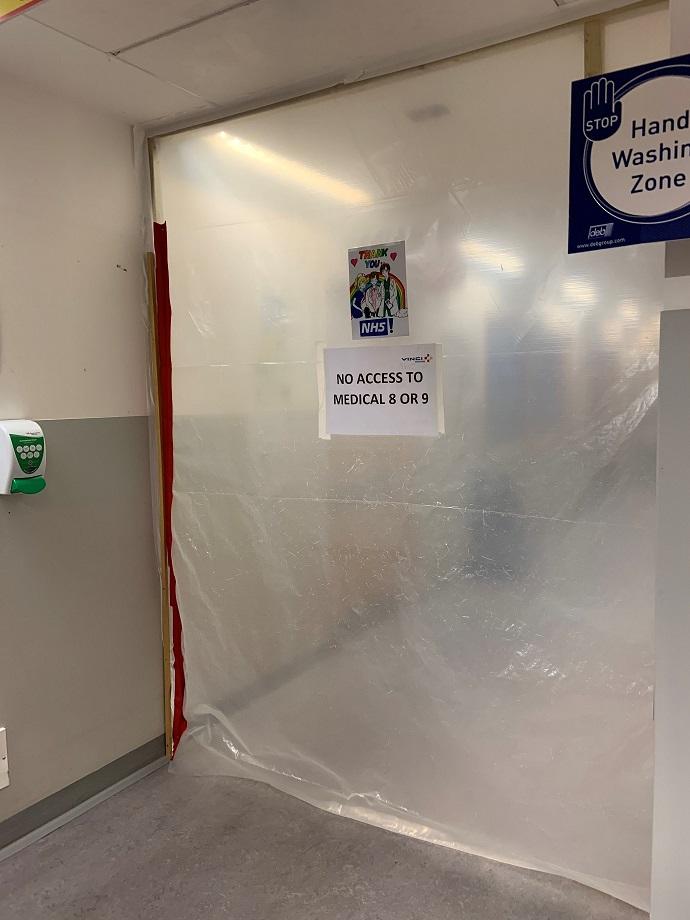
When I returned to haematology at the beginning of June, we had several new diagnoses of blood cancers. It is hard to know if these patients were presenting to healthcare professionals later because of the lockdown, but it certainly felt like there were some people who had been suffering with their symptoms at home for a while. It was a bit of an adjustment for me to go from being in a COVID setting to a completely ‘COVID secure’ ward. Our haematology inpatients are some of the most vulnerable to infection in society and therefore we were all doing our upmost to shield them. All staff started to be screened for COVID weekly and all visitors had their temperature taken on arrival.
Overall, my experience of being a redeployed haematologist during the pandemic has been a positive one. The most striking thing has been the exceptional teamwork and everyone pulling together for a common cause despite the difficult circumstances. There were definitely tough days and a lot of loss and difficult conversations but my lasting memories will be of the resilience of the staff within the NHS and amazing ability we have to come together for the good of the patients in their time of need.







